Sickness absence is only the visible tip of workforce health costs. Beneath it lies a far bigger drain on budgets and performance – from presenteeism to unmanaged chronic risks. This article explores what’s hidden, why it matters, and how employers can finally measure it.
Why absence data doesn’t tell the whole story
Most organisations rely on sickness absence to judge workforce health because it’s familiar, easy to report and appears objective. But absence only reflects a health issue once it has become severe enough to keep someone away from work. Long before that point, productivity, focus and energy are already affected – and those impacts rarely show up in traditional reporting.
UK employers are already absorbing significant direct health costs. Estimates suggest sickness now costs businesses around £103 billion each year, and average absence has reached 9.4 days per employee – the highest level in over 15 years1 2. Yet this still reflects only what is captured through absence reporting, not the much larger cost of working while unwell.
To understand the real financial impact of workforce health, employers need to look below the surface at what’s influencing performance before absence ever occurs.
Applying the iceberg metaphor to workforce health
Sickness absence is the part everyone sees – just like the tip of an iceberg above the waterline. It’s visible, measurable and often assumed to represent the whole problem. But absence is only the moment a health issue becomes too significant to ignore. The real drain on productivity happens earlier.
Beneath the surface lies a much larger mass of hidden costs. These can include:
- Early-stage health risks
- Gradual declines in stamina or concentration
- Chronic conditions without clear symptoms
- Mental health strain that hasn’t yet reached a crisis point
None of these typically prevent someone from working, but they silently reduce performance for months or even years. Presenteeism alone is estimated to result in an average of 44 lost working days per employee each year, making it one of the most expensive and least visible drains on productivity1.
The unseen portion matters most because it lasts longer and affects far more people. Many employees will never take long-term absence, instead working at a fraction of their capacity due to unmanaged health issues. The impact accumulates gradually, without triggering HR processes or being captured in absence metrics.
Absence is the point a health issue becomes visible. The real cost comes from everything that happens before that point.
Uncover hidden productivity costs
Discover how unseen health risks affect your bottom line and learn how to build a strong business case for early intervention.
How the iceberg looks in practice
Above the waterline – costs employers can see
- Recorded sick days
- Occupational health referrals
- Insurance claims
- Sick pay and cover for absence
These represent the final stage of a health problem.
Below the waterline – much larger costs employers rarely measure
- Reduced focus, stamina and decision-making
- Presenteeism due to pain, fatigue or stress
- Chronic risk developing without symptoms
- Early MSK strain affecting comfort and performance
- Turnover linked to ongoing stress or health pressure
- Energy dips affecting daily output
These are the slow, quiet and preventable costs that drain budgets without being logged.
What reactive data fails to capture
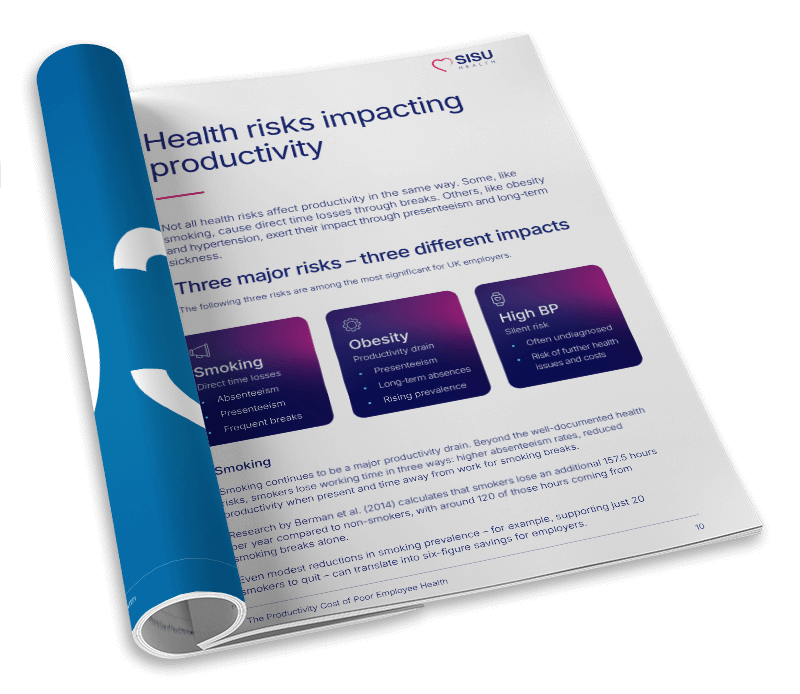
Presenteeism
Employees are physically present but working at reduced capacity due to discomfort, mental strain or low energy. This rarely triggers a system alert yet consistently undermines productivity.
Chronic risks without symptoms
High blood pressure, metabolic risk or early MSK strain can feel insignificant to employees, even as they chip away at stamina, sleep, clarity and immune resilience. Without early action, they turn into long-term conditions that are expensive to treat.
Mental health strain
Stress initially affects focus, emotional regulation and cognitive load – long before it becomes absence. By the time someone reaches burnout, they may have been under strain for months.
Health-driven turnover
When people struggle with ongoing health issues without support, they often leave environments that feel too demanding. Hiring replacements is expensive, but turnover is rarely attributed to underlying health pressure.
How organisations underestimate the true financial impact
Leaders want to make informed decisions, but without visibility of early health risks, even well-intentioned strategies can miss where the real cost lies. The result is an understated business case for prevention and a reliance on reactive spending.
Reliance on lagging indicators
Most organisations measure health only when it becomes a problem: sickness absence, claims data, GP referrals or Employee Assistance Programme (EAP) uptake. These are lagging indicators – they react to what has already happened. By using only backward-looking data, organisations end up funding treatment rather than prevention.
No visibility of early risk
Without population-level insights, early changes in blood pressure, metabolic risk, stress indicators or MSK strain are impossible to quantify. Leaders are left planning in the dark. They can sense that performance is being affected, but they can’t measure the cause, scale or cost.
Prevention seems optional
If leaders can’t see emerging risk trends, investment in prevention is easily deprioritised – especially during budget pressure. Wellbeing then becomes framed as a “benefit” rather than a cost-avoidance strategy. Without measurable insight, even valid initiatives struggle to win support.
Budgets default to reactive spending
This cycle leads to higher long-term costs. Money goes into treatment pathways, referrals, sick pay, recruitment to replace lost staff and extended HR support – expenses that could have been mitigated earlier with lower-cost interventions. The business ends up paying more, not less.
When organisations only measure health at the point of absence, they forfeit the opportunity to reduce cost before it appears.
Turning workforce data into strategic action
Reliable health insights enable leaders to make decisions based on risk, not assumptions. With measurable early data, employers can finally answer critical questions.
- Where are our biggest risk concentrations?
- How are different roles, departments or locations affected?
- Which health issues are influencing productivity before absence?
- What is the estimated financial impact if risks are left unaddressed?
Having this level of clarity transforms wellbeing from a discretionary initiative into a financially driven strategy.
Better targeting of investment
When organisations know, for example, that metabolic risk is highest in a specific operational team, or that stress scores are elevated in a seasonal function, they can invest precisely where it matters – rather than spreading resources thinly across the entire workforce.
Measuring outcomes over time
If employees continue to check in regularly, health patterns become measurable over months and years. Leaders can see whether risk categories are shifting, whether interventions are driving improvement, and which policies require review. This closes the loop on ROI.
Building a defensible business case
With visibility of where costs are emerging and how they are trending, HR and wellbeing leaders can present a quantified business case to senior stakeholders. Budget approval becomes simpler: decisions are based on hard data, not sentiment.
SISU Health helps leaders see the full picture
At SISU Health, we enable organisations to see beneath the surface of workforce health by making early risk measurable in a fast, accessible and ethical way.
Private, self-service health checks
Employees complete medically certified screenings in minutes, without appointments, clinical staff or barriers for shift workers. This increases participation across all demographics and job roles.
Immediate digital results and support
Results are available instantly via the SISU Health app and online portal, giving individuals a clear understanding of their own health – along with guided tools and resources that encourage long-term improvement.
Aggregated insights without identifying individuals
For employers, SISU Health converts thousands of individual health check results into anonymised, population-level insights. Leaders can spot trends in blood pressure, metabolic risk, MSK strain, lifestyle indicators of stress and more – without accessing any personal data or sensitive records.
Visibility that leads to action
Seeing risk concentrations allows organisations to:
- Prioritise support where the impact will be greatest
- Reduce reliance on reactive health costs
- Model potential cost avoidance
- Track measurable improvement over time
This brings confidence to decision-making and makes prevention financially credible.
Ultimately, SISU Health helps organisations take action before absence – where the greatest cost savings sit.
Make early health risk measurable
If you’re exploring how to embed prevention more effectively, the most useful next step is to see how early risk can actually be measured. Our team can walk you through our solution, show how workforce-level insights are generated, and discuss how SISU Health supports prevention before absence occurs.
Sources
- Lawrence, K., Pennycook, M., Hatfield, I., & Finch, D. (2023). Health and Prosperity: Addressing the impact of poor health on the UK economy. Institute for Public Policy Research (IPPR). Available at: https://www.ippr.org/research/publications/health-and-prosperity
- CIPD & Simplyhealth (2025). Health and Wellbeing at Work Survey Report 2025. Chartered Institute of Personnel and Development. Available at: https://www.cipd.org/uk/knowledge/reports/health-well-being-work/

Ready to deliver visible, measurable workforce wellbeing?
Discover how we help employers build healthier, more productive workforces.